Presentation
A 25-year-old white male patient reported dryness and irritation with contact lenses in both eyes. He had been wearing contact lenses for 8 years, and over the last 3+ years the lenses had become increasingly uncomfortable. At the time of his visit, he could not wear the lenses for more than 6 to 8 hours before discomfort set in, and his eyes felt dry and therefore uncomfortable for the rest of the wearing day. He had been prescribed a variety of artificial tears (which he used frequently), lubricating ointments, topical cyclosporine, even punctal plugs, but nothing sufficiently helped.
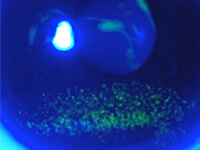
The patient had previously been noted to have a nocturnal lagophthalmos and a history of inferior corneal staining that did not resolve with periodic cessation of lens wear. His job required him to drive 3 to 4 hours every day.







